Hits: 54
Enjoying this newsletter? Why not share it with a friend? A rough flu season may be taking shapePlus updates on measles, infant botulism, the question grab bag and good news.
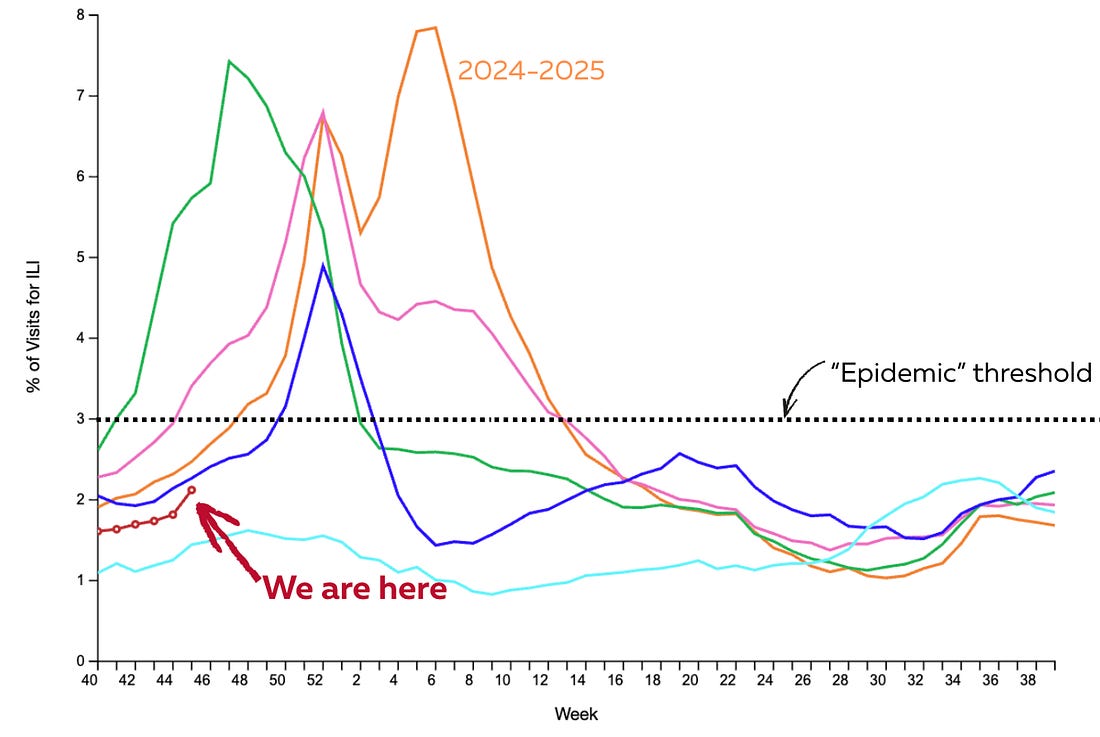
The government shutdown is over, and a few things are finally back online: CDC data, SNAP funding, and flights returning to something resembling normal (or at least as “smooth” as air travel ever gets). That’s the good news. The bad news? We could be heading into a brutal flu season. The infant botulism outbreak linked to formula is climbing, and the U.S. may soon face a review of its measles elimination status, following Canada’s loss of theirs last week. And with the gears turning again in Washington, health policy questions are back in play. One we got recently: was the Affordable Care Act ultimately helpful or hurtful? (See our answer below.) As always, we’ll end with some good news. Infectious disease “weather report”Every Friday, the CDC updates their “influenza-like illness” (ILI) data. This is a database where providers tally patients who presented with ILI—a fever, a cough, and/or sore throat—at their offices. So these numbers are a general indication of the climate of respiratory health in the United States. ILI is starting to creep up (particularly in Louisiana and Southern states) but is still below the “epidemic” level threshold. (This threshold is usually when I put on my mask when I’m at airports or crowded indoor places, because I don’t have time to get sick.) In other words, things aren’t bad yet.
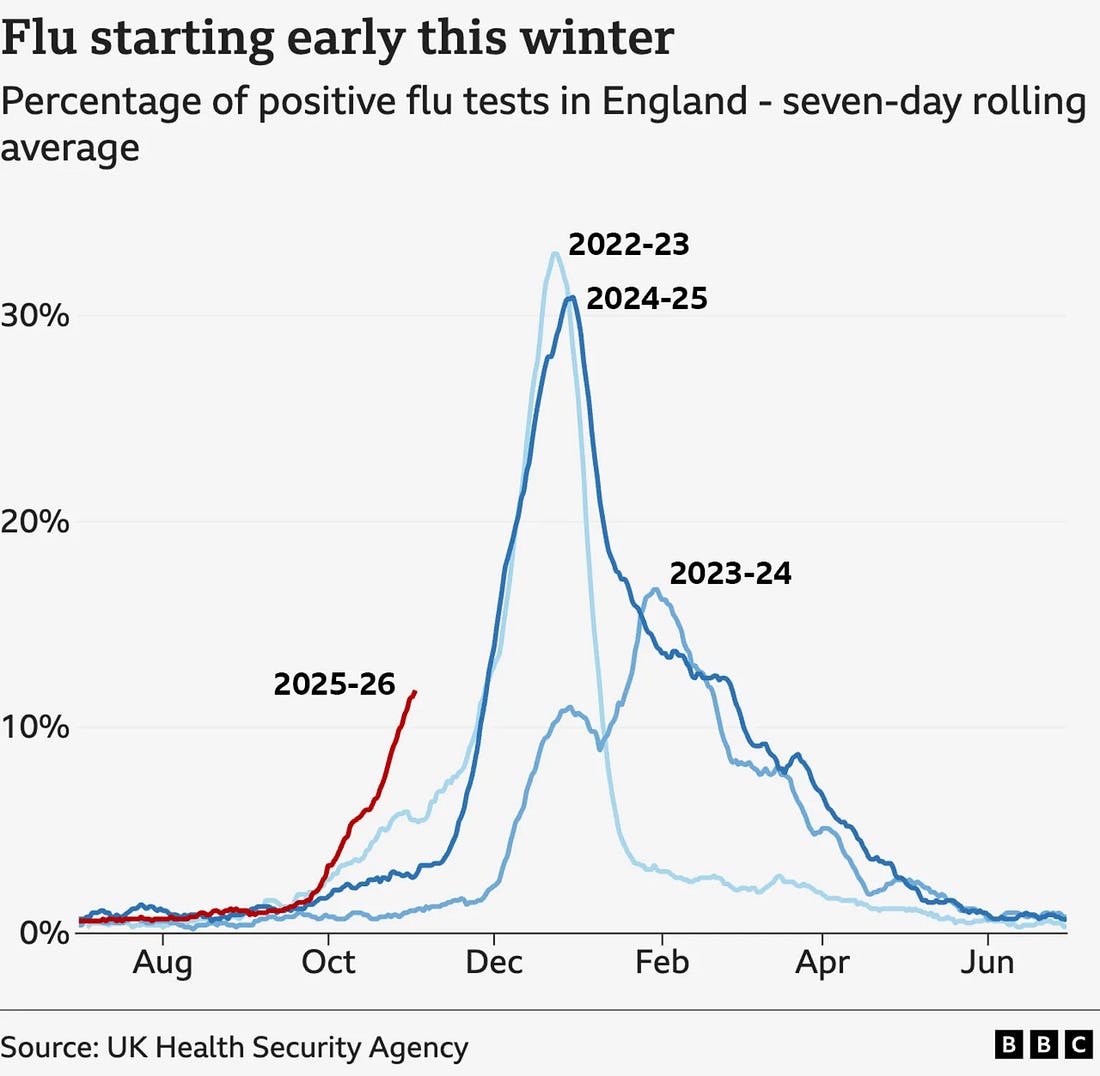
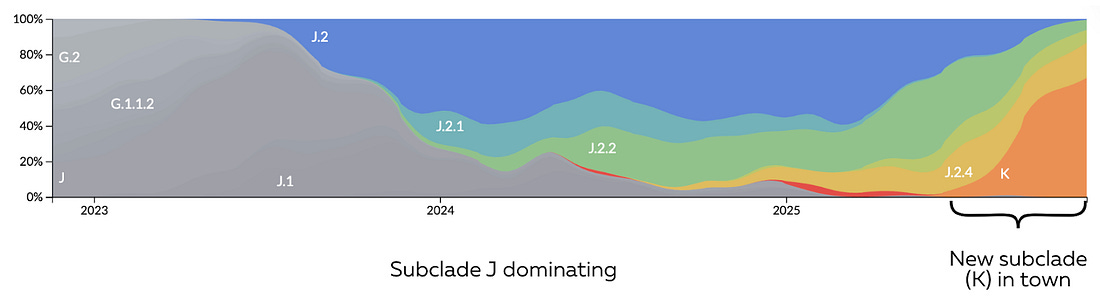
ILI rates in the United States. Source: CDC; Annotated by Your Local Epidemiologist FluThat said, buckle up for a potentially rough flu season. While the U.S. season is just ramping up, the U.K., Japan, and Canada are already seeing steep increases. Why? One strain of flu—influenza A (H3N2)—mutated over the summer as it spread through the southern hemisphere. Specifically, it shifted from a J subclade to a K subclade.
H3N2 subclades over time. Source: Nextstrain.org; Annotated by Your Local Epidemiologist Mutations are normal for the flu. In fact, the flu is infamous for quick, unpredictable curveballs. But this particular change raises concern for two significant—but not catastrophic—reasons:
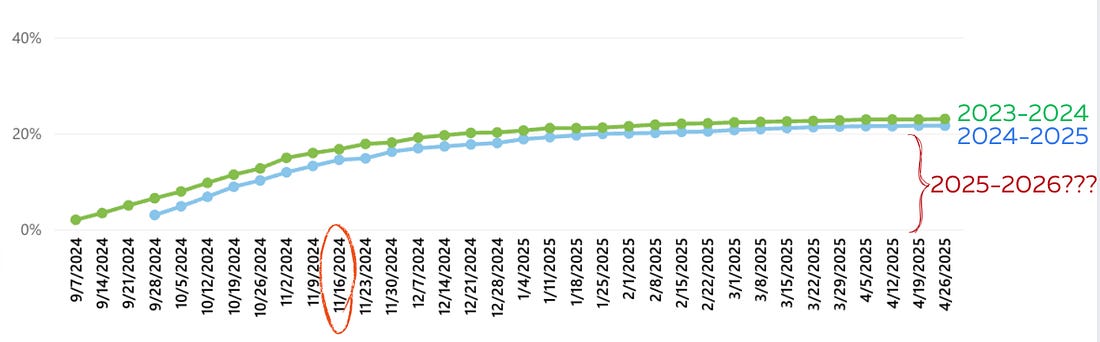
Together, these factors mean the virus will be better at slipping past both vaccines and prior immunity. That likely translates to more cases and more severe disease among those at highest risk. Flu doesn’t behave uniformly around the globe. One strain may dominate in one region while a different strain circulates elsewhere. So what happens abroad doesn’t always predict what happens here. However, updated CDC data shows that while flu is still low, it’s growing and the strain that is dominating spread (51% of U.S. flu samples) is this newly mutated flu virus (called H3N2 subclade K). In other words, the same strain behind surges in the U.K., Japan, and Canada is already taking off here, too. But we’re far from powerless. Vaccination still matters—a lot. U.K. data shows it reduces hospitalization by 70-75% in kids and 30-40% in older adults, and it protects against other circulating flu strains. (This year’s vaccine is important enough that the U.K.’s National Health Service launched a nationwide “flu jab SOS” campaign.) We use slightly different vaccines in the U.S., so the numbers may not be quite this high, but still it will provide some protection. What this means for you: This is the perfect time to get the flu vaccine. Also, flu tests will still be able to pick up this strain, and and if you do get sick, early antiviral treatment like Tamiflu can help reduce the number of days you’re sick. RSVRSV activity continues to increase among our youngest. We’ve heard from some of you that the RSV vaccine isn’t stocked everywhere. After checking with Vaccines for Children, there are no national shortages—meaning some pediatric practices are simply under-ordering due to underestimating demand. Covid-19We’re in a Covid lull, which is great. Historically, Covid cases start ticking up by the end of November due to changing weather, holiday travel, and indoor gatherings. One big question right now: are vaccine rates lower this year because of the federal disarray under RFK Jr.? Normally, we’d have clear national data by now. But the CDC website hasn’t been updated yet—I’m hoping that’s due to the government shutdown, not anything more concerning (like malice).
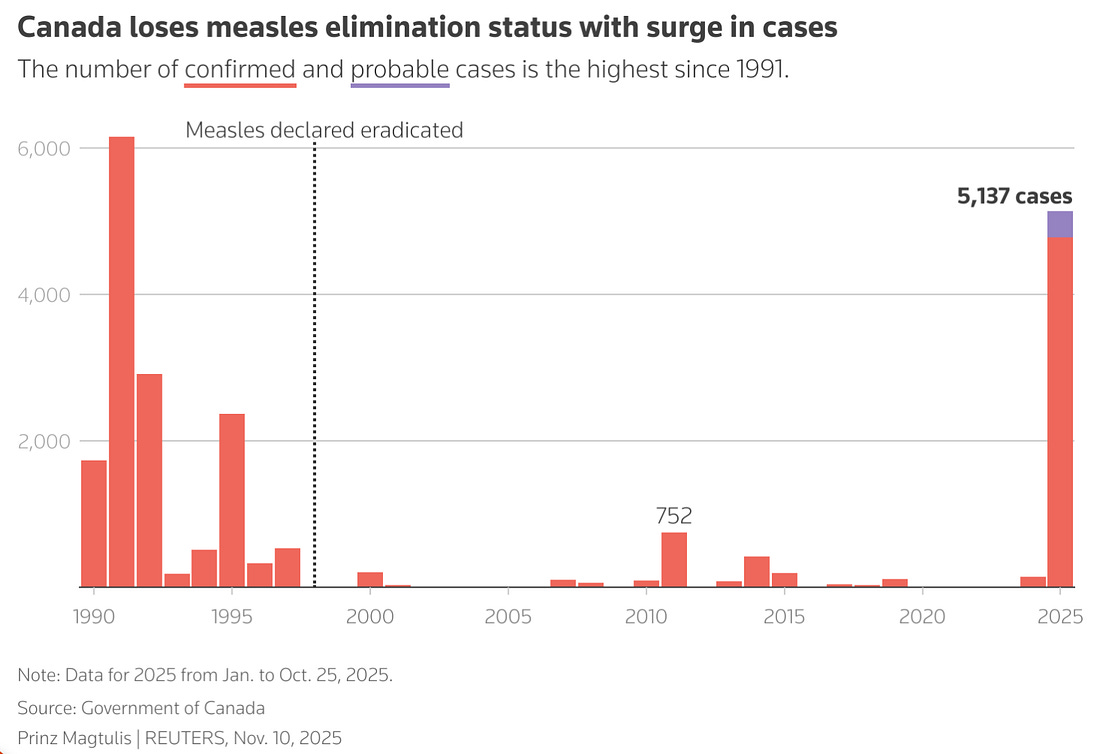
Covid-19 adult vaccination rates, United States. Source: CDC; Annotated by Your Local Epidemiologist These numbers matter. Without them, we can’t accurately anticipate what’s coming: hospital strain, missed work, and the broader burden of a potential wave. State data give us a glimpse, though, and it’s not reassuring. New York, for example, is reporting vaccine uptake about 30% lower than this time last year. MeaslesCanada lost its WHO measles elimination status last week after the same strain circulated there for more than a year, resulting in more than 5,200 cases and 2 deaths (89% of cases are unvaccinated). This is their worst year since 1991. Losing this status means that measles is now considered “endemic;” in other words, it’s constantly spreading across the country and not due to travel. This is a concern for people who are unvaccinated, including parents of children under 12 months old, who are too young to get the vaccine. What does this mean for the U.S.? The Pan American Health Organization—the World Health Organization’s regional office for the Americas—will review the U.S. status in January. We’ve also seen the most annual cases (1,600+) since 1990. But elimination status isn’t determined by total case count—it depends on whether a single strain spreads continuously for 12 months. In other words, it requires sustained transmission of one outbreak, not multiple separate outbreaks seeded by travel. We don’t yet know whether the U.S. meets that threshold, and I’m looking forward to seeing the PAHO’s assessment. One interesting feature of measles is its natural pattern: it tends to surge every five years, even before vaccines existed. Are the Americas just having a bad year? Possibly, but it’s likely a mix of both a bad year and a broader problem: declining immunization rates. A severe human case of bird fluAfter nearly nine months without a human case—and with very little activity in birds—bird flu is picking up again. A person in Washington State, right along a major migratory bird pathway, has developed a severe infection. Details are still sparse, but the leading hypothesis is exposure to backyard poultry that had contact with wild birds. This is the first human case ever reported with the H5N5 strain—a different strain from H5N1, which has caused roughly 70 human cases since the beginning of last year. If you have backyard flocks, you are at increased risk for bird flu infection, and it can be severe. Take appropriate measures, especially now that bird flu is starting to ramp up again and we really don’t want to give this virus an opportunity to jump, mutate, and create another pandemic. Botulism outbreak update: 23 reported infant casesMore infant botulism cases linked to ByHeart formula were reported last week, bringing the national total to 23. While the company ultimately recalled all of its products, its initial response—pushing back on regulators and downplaying the evidence—badly misfired. And the evidence was unusually clear:
This is the first time this bacteria has ever been detected in infant formula. Typically, infant botulism comes from environmental exposure or honey. And because symptoms can take up to 30 days to appear, epidemiologists expect the case count for this outbreak to grow. Two families have already filed lawsuits. What this means for you:
The communication lesson: ByHeart’s early messaging—insisting the recall was simply “out of an abundance of caution,” hinting at consumer error, and minimizing the link—created confusion, frustration, and mistrust among parents. It’s a textbook example of what not to do, and I hope it’s taught in classrooms in years to come: When the facts are pointing in one direction, denying them only deepens public concern and hurts the trust of a brand. As New York YLE Marisa wrote in her moving piece last week, infant botulism is traumatic for families. Shame and blame have no place here. Shutdown is over, but SNAP impacts remainThe government shutdown ended with a commitment to fully fund the Supplemental Nutrition Assistance Program (SNAP) through September of 2026. That’s a welcome relief. But the disruption left wide-ranging effects that can’t be fixed with a check alone. A clinician and YLE reader shared stories from the field highlighting how deeply SNAP supports long-term health—and how quickly progress can unravel when those benefits are interrupted.
Bottom line: People’s trust in the safety net is ruptured, with potential long-term effects to health and disruptions to treatment plans. To be clear, food banks stepped UP during the shutdown. But sometimes, food banks and pantries can’t fully replace the choice, consistency, and nutritional quality that SNAP provides. Good news: politics, make room for epiPublic health has often viewed politics as the third rail: Don’t touch it lest you get burned. The problem with this is that it ignores the fact that the third rail provides power to the train. I’m cheering on my fellow epidemiologists who are running for political offices, as reported in The Atlantic. Question grab bagI loved yours and Hayden’s piece on the “5 ways the health care system is utterly insane.” But I have a simple question: Was Obamacare helpful or hurtful? Short answer: Both. When Obamacare (or the Affordable Care Act), became law, it changed American health care in ways that were both dramatic but also imperfect. Millions of people gained insurance through Medicaid expansion or subsidized marketplace plans, and protections like coverage for pre-existing conditions, no lifetime limits, and free preventive care became reality for many families. Suddenly, going broke from a hospital visit was less common, and young adults could stay on their parents’ plans longer. But the story isn’t all victory. Costs remain high for all. People in states that didn’t expand Medicaid were left behind, and navigating the system—marketplace rules, subsidies, enrollment windows—is a maze. This also didn’t touch consolidation or the underlying drivers of cost. In short, Obamacare helped a lot, giving millions their first real protection and peace of mind, but it didn’t solve the underlying chaos of U.S. health care. Bottom lineEnjoy the viral lull, as more will come soon! Love, YLE Your Local Epidemiologist (YLE) is founded and operated by Dr. Katelyn Jetelina, MPH PhD—an epidemiologist, wife. YLE is a public health newsletter that reaches over 400,000 people in more than 132 countries, with one goal: to translate the ever-evolving public health science so that people are well-equipped to make evidence-based decisions. This newsletter is free to everyone, thanks to the generous support of fellow YLE community members. |