Hits: 88
|
 |
Enjoying this newsletter? Why not share it with a friend?
A flu surge, NYC overdose decline, and a mental health services shake-up
Your weekly Dose as we head into Thanksgiving.
|
|
|
|||||||||||||||
There’s a lot to cover before the holiday next week, so let’s jump right in.
Infectious disease “weather report”
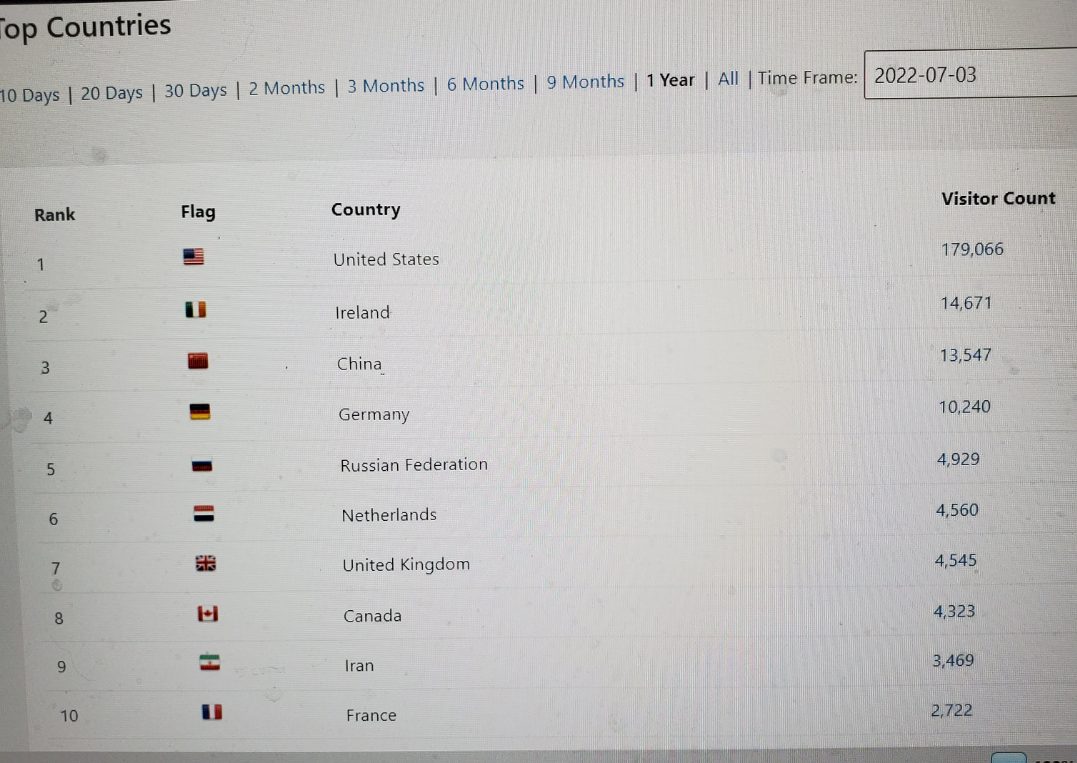
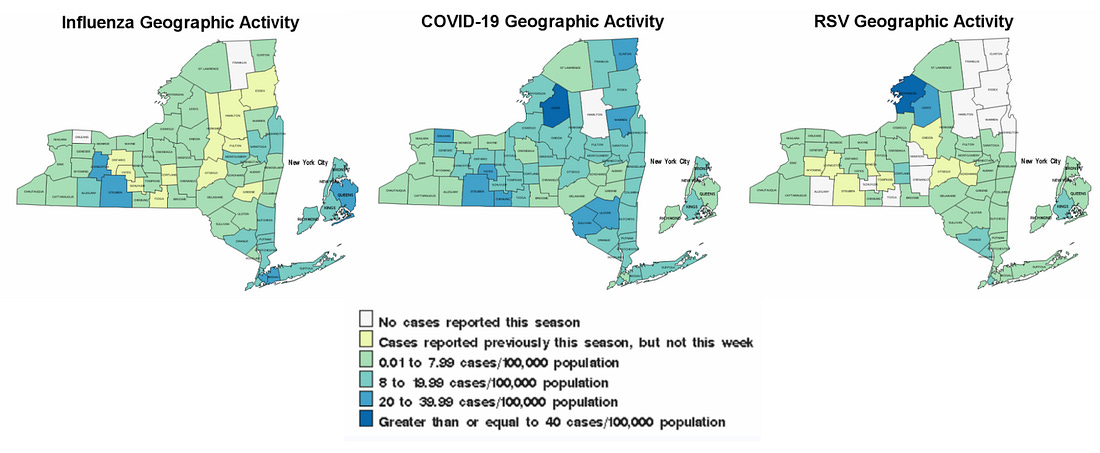
Flu: Flu is increasing quickly. The most recent data show that cases and hospitalizations in the state have increased by 78% and 53%, respectively. In NYC, emergency department visits for the flu rose by 104%.
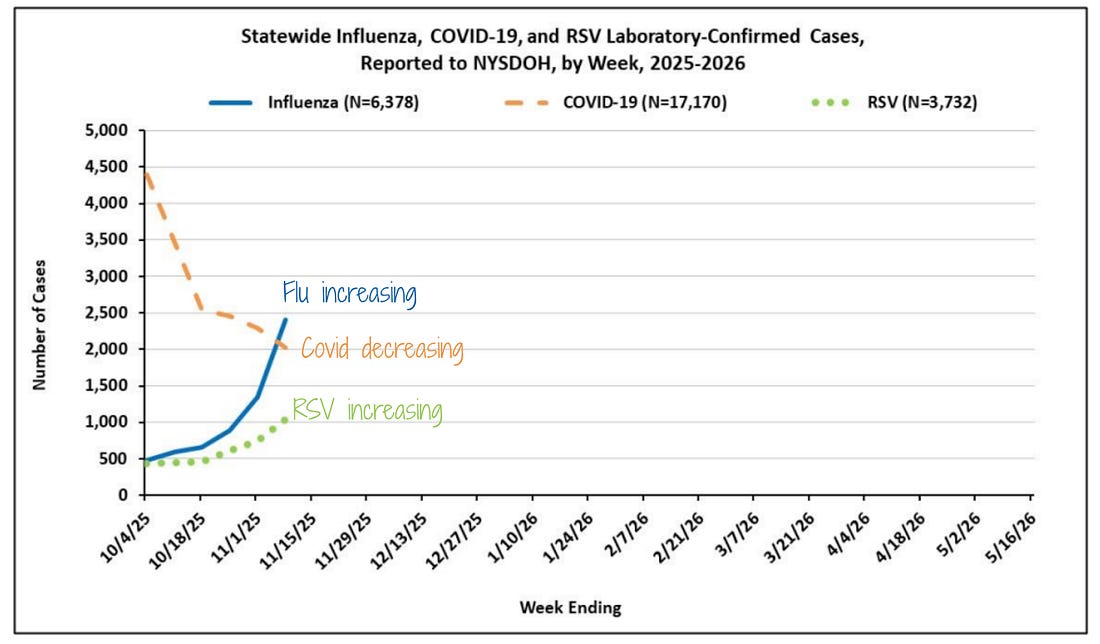 |
Cases of respiratory viruses in New York. Figure from the NYSDOH Respiratory Surveillance Report.
Earlier this week, YLE National reported on a new flu virus mutation that could potentially lead to a bad flu year in the U.S. We don’t know exactly how things will play out, but the bottom line is that flu vaccination remains our best protection.
RSV: Also increasing across the state and in NYC, mostly in kids under 4. Statewide, hospitalizations increased by 70%, while emergency department visits in NYC went up by 40%.
Covid-19: Cases and hospitalizations are decreasing in both NYC and across the state.
 |
Cases of respiratory viruses by New York county. Dark blue areas have the highest case rates. Figure from the NYSDOH Respiratory Surveillance Report.
As we head into Thanksgiving, when many of us will be traveling to see loved ones, flu and RSV are top of mind. To reduce the spread of illness, consider masking in indoor crowded spaces—I’ll be wearing mine on the train and in the airport—and reducing contact with others if ill.
Good news: Overdose deaths are declining in NYC—but progress is uneven
For the first time in years, NYC saw a significant drop in overdose deaths—a 28% decrease last year from 2023—but that still totals 2,192 deaths: far too high.
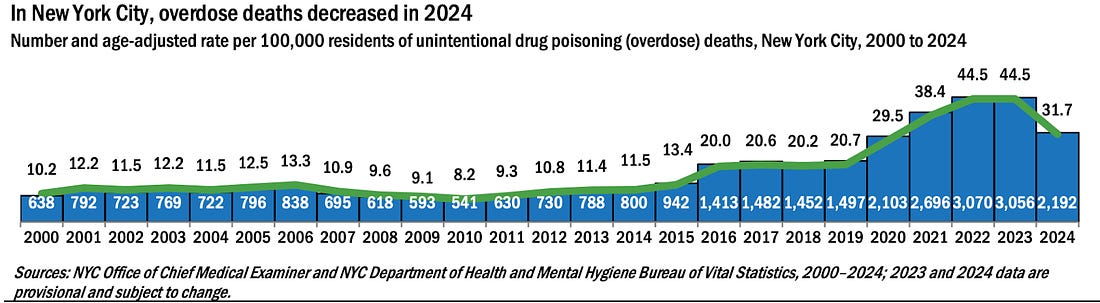 |
Figure from the NYC Department of Health and Mental Hygiene.
Last year, 78% of overdose deaths in NYC involved an opioid, a reduction from 83% in 2023. Fentanyl remains the leading driver, involved in 73% of deaths, but that’s also down from 80% in 2023.
One success story is Staten Island, which saw the steepest drop in overdose deaths.
A possible reason: the implementation of a hot-spotting strategy. Officials analyzed emergency medical services (EMS) and hospital data to identify where overdoses were happening most. Then they deployed peer counselors to those areas with the life-saving opioid overdose-reversing medication naloxone (also known as Narcan), support services, and treatment referrals.
Over the summer a hot-spotting program based off of Staten Island’s was launched in the Bronx as well. This is greatly needed as the Bronx still has the highest overdose death rate compared to other boroughs. I’ll be keeping an eye on the program’s progress and any outcomes reported.
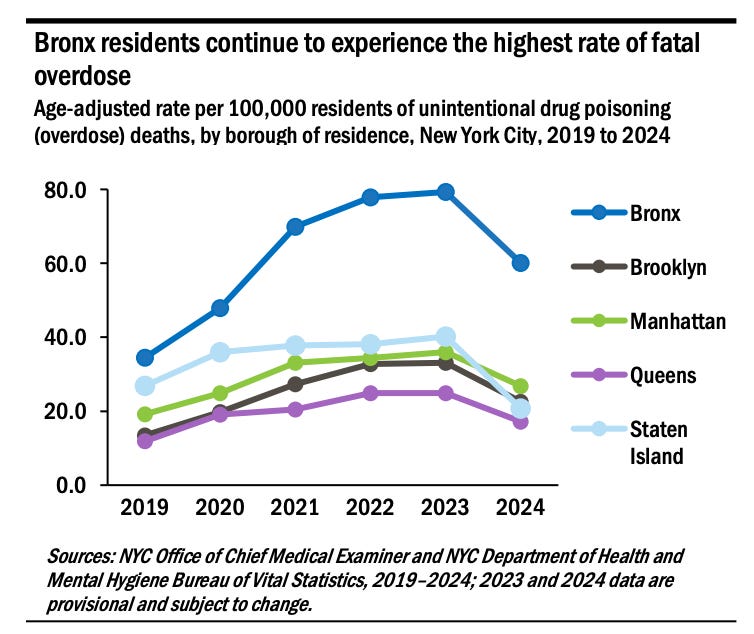 |
Figure from the NYC Department of Health and Mental Hygiene
Despite the encouraging drop, overdose is still a leading cause of premature death in NYC.
And huge inequities still exist. Overdose deaths in black and Latino New Yorkers remain about twice as high as the rate among white New Yorkers.
There are still actions we can take to continue to reduce the risk of overdose death amongst our fellow New Yorkers:
Carry naloxone (Narcan).
- All New Yorkers can receive free naloxone and training from registered Opioid Overdose Prevention Programs (OOPPs) on how to recognize the signs of an overdose and administer the medication.
- Health Department vending machines: Locations can be found on this page.
- Over-the-counter naloxone at pharmacies: Available without a prescription at most major chains (map here).
- Most insurance providers will cover all or part of the cost of naloxone, and New York State will cover copayments of up to $40.
There is also a hotline for individuals seeking support or treatment for substance use for themselves or their loved ones. Call or text 988, or visit the 988 website for 24/7, confidential support.
Changes to the B‑HEARD program (iN AMBULANCE RESPONSE TEAMS IN NYC)
Last week, Mayor Eric Adams announced a shift to B-HEARD—the Behavioral Health Emergency Assistance Response Division, a pilot program launched in 2021 to respond to 911 mental health emergency calls with trained medical and mental health teams.
Under the new model, teams will move from two emergency medical technicians (EMT) and a social worker to one nurse, a social worker, and an ambulance driver—all employed by NYC Health + Hospitals.
These teams are dispatched in cases of nonviolent but urgent behavioral health crises: suicidal ideation, substance misuse, acute mental health episodes, and similar situations.
In the triage process, 911 operators route mental health‑related calls based on criteria around safety and risk. If a situation is assessed as nonviolent and primarily behavioral health driven, it may be routed to B‑HEARD instead of the traditional law enforcement/emergency medical services (EMS) response. The program operates in Northern Manhattan, the Bronx, Central and South Brooklyn, and Western Queens, from 9 a.m. to 1 a.m.
Let’s give it a closer look.
Why does this program exist?
Historically, almost all mental health 911 calls in NYC were routed to the New York City Police Department (NYPD), sometimes alongside basic EMS responders. Some experts argue that this approach often lacks the de‑escalation skillset, therapeutic lens, and follow‑up needed for mental health emergencies.
There is evidence that when police are first responders in a mental health crisis, outcomes can be worse: individuals in crisis may feel criminalized, unsafe, reluctant to seek help, and in worst cases may face use of force. For example, in the U.S. people with untreated serious mental illness are estimated to be up to 16 times more likely to be killed by law‑enforcement during an encounter.
By deploying mental or behavioral-centered teams, B‑HEARD tries to reduce unnecessary police involvement, deliver more appropriate care at the scene, and connect people to community‑based follow‑up.
Has B‑HEARD been effective so far?
A city comptroller audit earlier this year found the program is promising in concept but hard to evaluate due to limited data and implementation gaps.
Key findings:
- Between fiscal years 2022-2024, B-HEARD covered 96,291 mental health-related 911 calls during operating hours.
- Only about 25% (just over 24,000 calls) resulted in a B-HEARD response.
- Around 60% were deemed ineligible (some due to safety concerns, others because no EMS operators were available to screen).
- Even among eligible calls, 35% never received a response for unknown reasons.
- Critical process steps (assessments, follow-up referrals) were often incomplete or not documented.
On the positive side, among clients surveyed, the results were strong:
- 99 % said they were treated with respect.
- 96 % said the team helped them.
In short, the idea is promising, but the current program lacks data to properly evaluate its effectiveness at meeting its goals.
Why the change?
New York faces a shortage of EMTs and paramedics and has long ambulance response times. By freeing up EMS workers for broader medical emergencies, the city hopes to improve ambulance response times across the city.
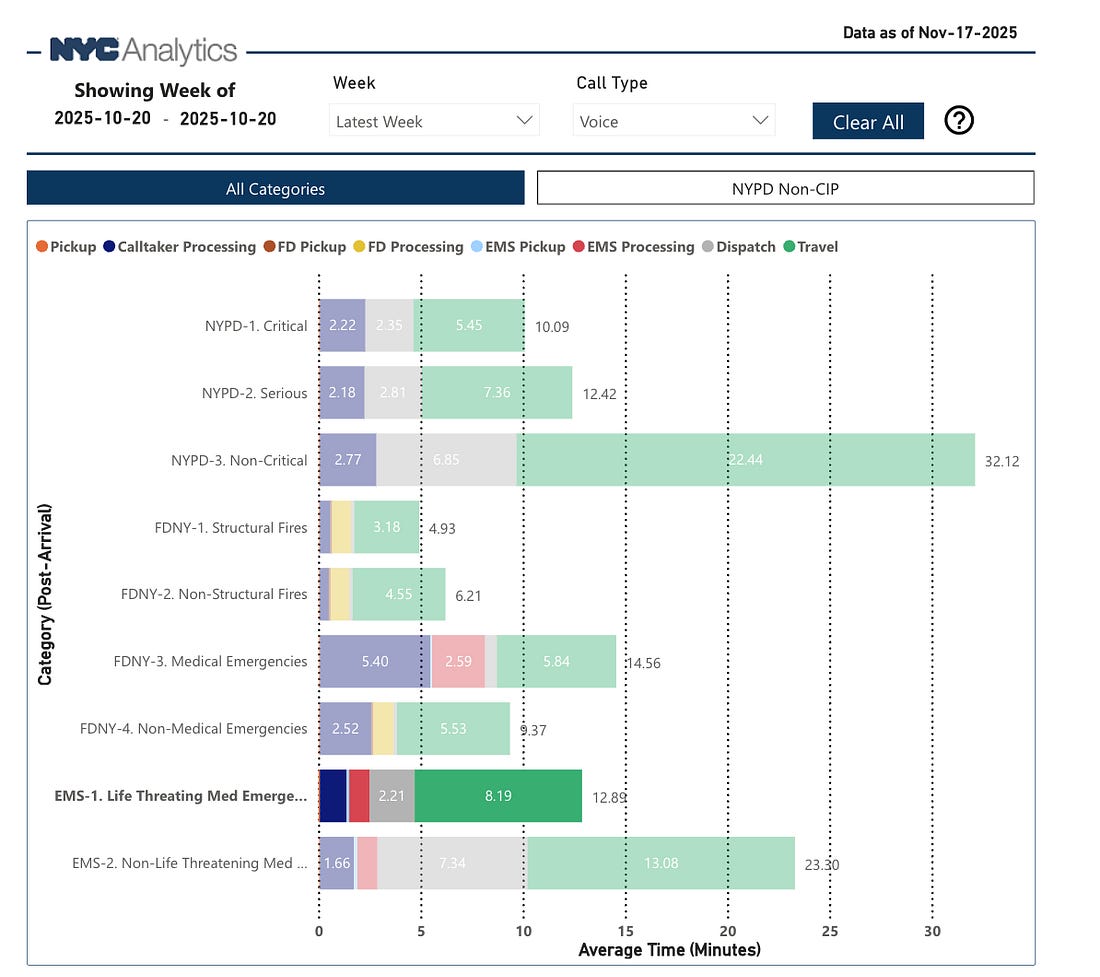 |
NYC average end-to-end response times for ambulances for life-threatening emergencies was 12 minutes and 53 seconds during the week of October 20 (the latest week available). Figure from NYC 911 reporting.
Importantly, during a behavioral health crisis, if additional medical backup is needed (e.g., someone becomes medically unstable), the driver/nurse team can summon an ambulance. The nurse offers stronger clinical capacity on‑scene than EMTs alone, potentially improving care and triage.
Looking ahead and my thoughts
With longer ambulance wait times, it’s a logical step to free up EMTs to shorten response times. And if there are enough nurses at NYC Health + Hospitals to redirect some to B-HEARD teams without disrupting hospital operations, having advanced medical support on the response teams could be beneficial. But the bigger question remains how effective this program has been at responding to mental health issues, while maintaining safety for those experiencing mental health crises and for first responders.
The other question at hand is the timing of this change. Mayor Adams has one more month on the job before Mayor‑elect Zohran Mamdani takes the helm on January 1st. Mamdani has signaled plans to expand B‑HEARD city‑wide beyond the pilot, and fold it into a new Department of Community Safety. Will these changes hold in Mamdani’s new administration? If not, will shoring up EMTs in NYC for one month make any real difference in ambulance wait times? Will the program go through another overhaul, potentially further limiting our ability to assess its effectiveness? These are the things I’ll be looking out for over the coming months, and I will report back with any updates.
Bottom line
As we head into the holiday, I’m feeling especially grateful for New York’s public health champions—the heroes and systems working behind the scenes to keep us safe. The encouraging decline in opioid deaths, expanded mental health outreach, and strong infectious disease surveillance systems are testaments to that.
To everyone working towards a healthier state: thank you for all you do. Your work makes New York better, every single day.
I’m wishing everyone a restful Thanksgiving—indulge in that pie, wear those stretchy pants, and I’ll see you after our break next week!
Love,
Your NY Epi
Dr. Marisa Donnelly, PhD, is an epidemiologist, science communicator, and public health expert. This newsletter exists to translate complex public health data into actionable insights, empowering New Yorkers to make informed and evidence-based health decisions.
Thanks for your financial support of Your Local Epidemiologist in New York! I couldn’t do this without you. — Marisa