Hits: 126
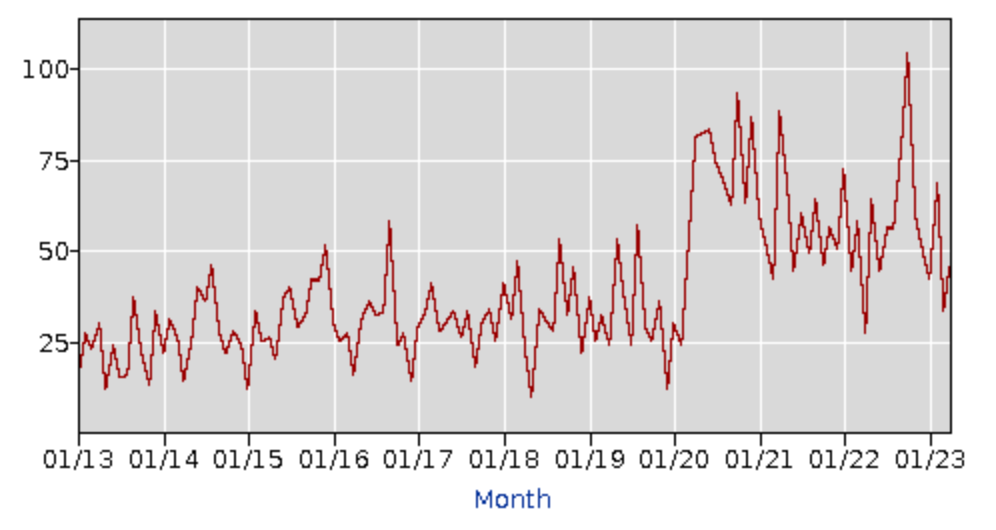
Later this summer, I’ll mark the one year anniversary of Force of Infection. As I think about the year that has passed and the second year ahead, I want to take a moment to explain why I write this newsletter. This past December, there was a period when everyone in my household except me was laid up with strep throat. Miraculously, I was spared—which earned me the privilege of overseeing four visits to the doctor’s office, five trips to various pharmacies, and the role of chief caregiver during multiple days out of school and work. On top of everything else, the antibiotics prescribed to treat my family’s bacterial infections were in short supply. The same inelastic supply chains that couldn’t provide enough masks and at-home tests during COVID-19 waves put common antibiotics in shortage. I had to make multiple phone calls to our doctor and various pharmacies to find a suitable replacement that was actually in stock. Even now, months later, certain amoxicillin products remains in short supply. If all this sounds familiar, it’s not just in your head. Similar dramas played out in millions of households this winter. Such is the nature of epidemics — it’s everywhere, all at once. And of course, it wasn’t just strep throat that went around. First RSV, then COVID-19, influenza, adenovirus, and finally stomach bugs all took turns making us miserable. It’s a carousel that families couldn’t seem to get off. Infectious disease activity has finally quieted down, but it was a tough school year (again) for many families. According to the Bureau of Labor Statistics, 2022 and the first months of 2023 were as challenging for childcare issues as the early years of the pandemic. Let me say that again: disruption to childcare has been ongoing for three straight years. In fact, October 2022 was the worst month for childcare issues across the entire pandemic, and this February was on par with pre-vaccine levels. Even last month, when both flu season and covid had died down, was worse than the height of flu season in the years before the pandemic. Not all of these childcare issues are attributable to illness, of course. But, given the successive waves of infections, I suspect that many are.
Labor Force Statistics: Employed with a job, Not at work, Childcare problems. BLS. The impact of these illnesses was felt not just in homes, but also in schools and workplaces. When kids are home sick from school, parents have to miss work to care for them. And even in households without small children, infections can wipe days or even weeks of work off the calendar. It creates a ripple effect, as businesses struggle to maintain productivity and people are forced to make impossible choices about how to keep all the balls in the air. The backlash to pandemic-era measures would have you believe that there are two modes: all or nothing. Either you spare no thought to what’s going around, or you “live in fear.” This is a false dichotomy. We can make decisions about avoiding infections just like we make any other decision about managing risk. There is a sustainable middle ground for staying healthy that I think is worth incorporating. When a storm is forecasted, I pack an umbrella or cancel plans at the park. When my budget is tight, I spend less. When I know there’s a lot of flu going around, I wear a mask on the metro. If I’m not feeling well, I work from home. For older adults or people with health conditions, precautions during flu season or a COVID-19 wave may be more strict. But without any awareness of what the current outbreak situation is, there is nothing to base sound decisions on. The first step is knowing what’s going around so you can adjust accordingly — and helping people access that information is one of the main goals of this newsletter. I want people to have quick, digestible information about what’s going around their communities so they can make those informed decisions. My hope is that readers will miss fewer days of work and school, need fewer trips to the doctors office or pharmacy, and enjoy overall better health. I also hope that if and when there is a severe public health event, you’ll have a place to turn for trusted information. As Your Local Epidemiologist and I wrote recently, public health did not always succeed at connecting with the public during the pandemic. “People do not turn to media companies for their news,” we wrote. “They turn to anchors and reporters whom they come to know and trust—warm bodies that they can relate to and who appear consistently over time. We don’t give the public enough opportunities to see and trust warm bodies in public health. Messages must be delivered by real people, preferably the same people, in a style that feels human.” I hope to do some of that here, too. So thanks for joining me here at Force of Infection. I hope you stick around for year two. Quick summary of outbreaks this weekCOVID-19 hospitalizations and deaths continue to decline. Trends in wastewater data are also stable. I’m watching the Southern region of the country most closely, as that is where previous summer waves have started. But so far there are no signs of increase. Influenza-like illness and RSV are still declining. We are now well out of flu season, thankfully. Norovirus is falling in all four regions of the country. Gerber Good Start formula has been recalled. This time of year, events like potlucks and block parties where food sits out in the hot sun too long are a big source of foodborne illness. FDA has some good tips for food safety when eating outdoors. One highlight is not to keep food out for more than 2 hours (or 1 hour if it’s more than 90 F outside). Also take care when handling raw meats. Mpox case counts remain low, but CDC is warning of a probable increase this summer. CDC has some good information about how to protect yourself from mpox, especially as we head into Pride month.
Photo by Laurentiu Iordache on Unsplash
|