Hits: 117

Happy New Year! I hope you had a restful holiday. Here is the latest on COVID-19, flu, and RSV in the U.S.
Overall respiratory health
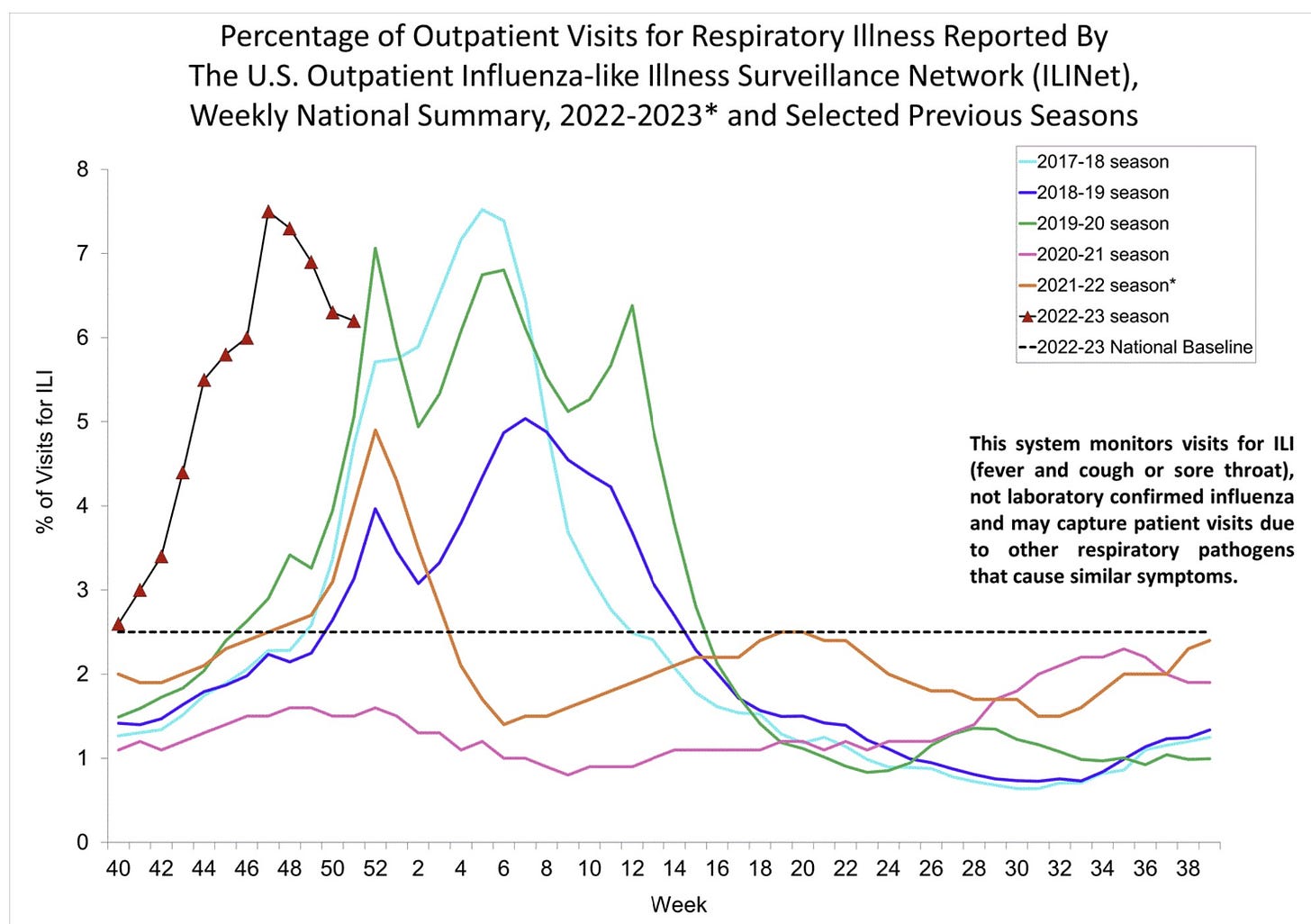
It’s still looking rough out there. High numbers of influenza-like illnesses (ILI)—fever, cough and/or sore throat reported at doctors’ offices—are peppered across the U.S.
Respiratory illness season was early and has already reached a high compared to the last decade, but it’s on the descent. It’s too early to celebrate, though, as we may see multiple wave humps as we did in the pre-pandemic years.
If we zoom into specific viruses, we see different stories.
RSV
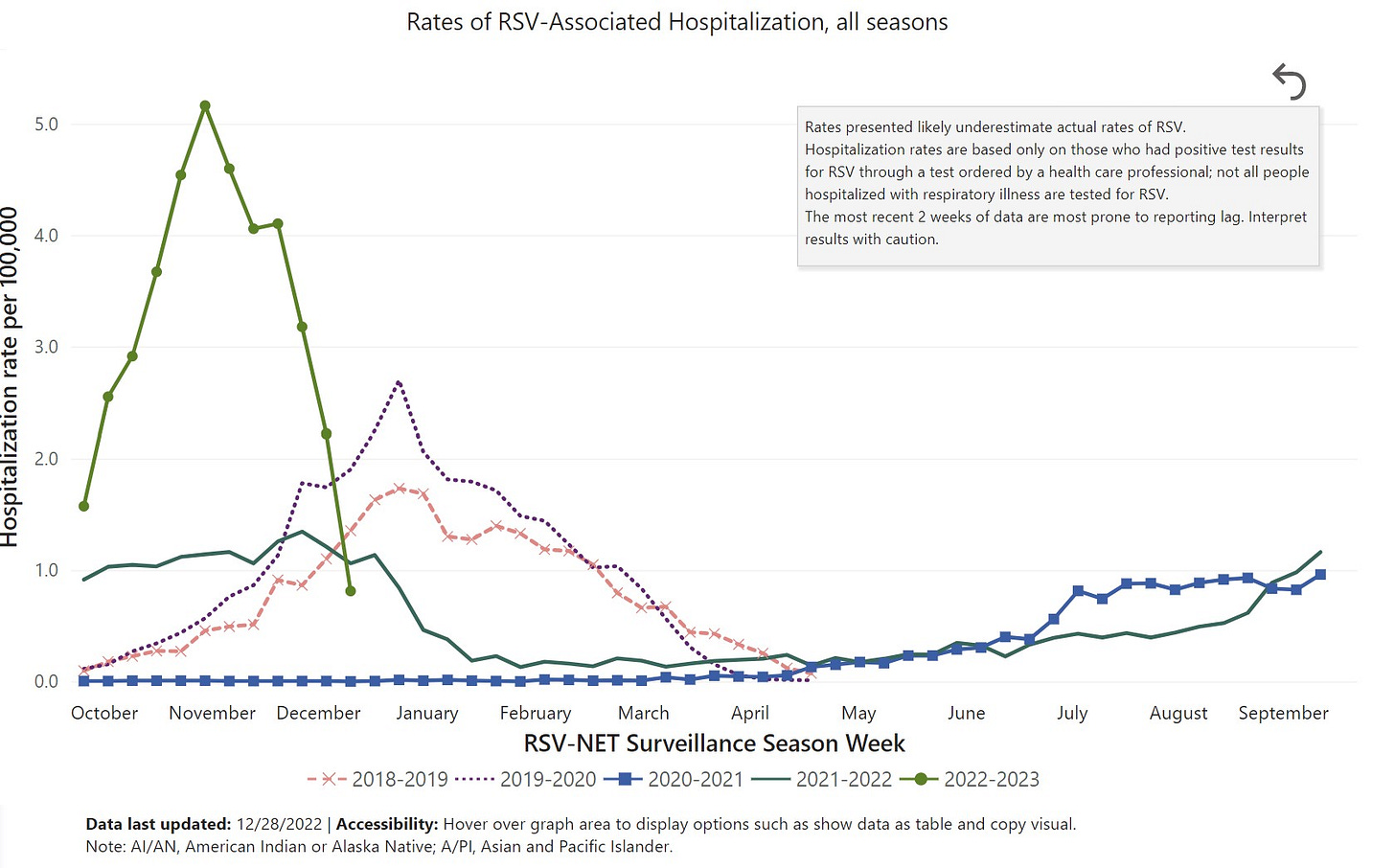
RSV is nosediving, a welcome development for older adults, parents of kids under 5, and pediatric hospitals.
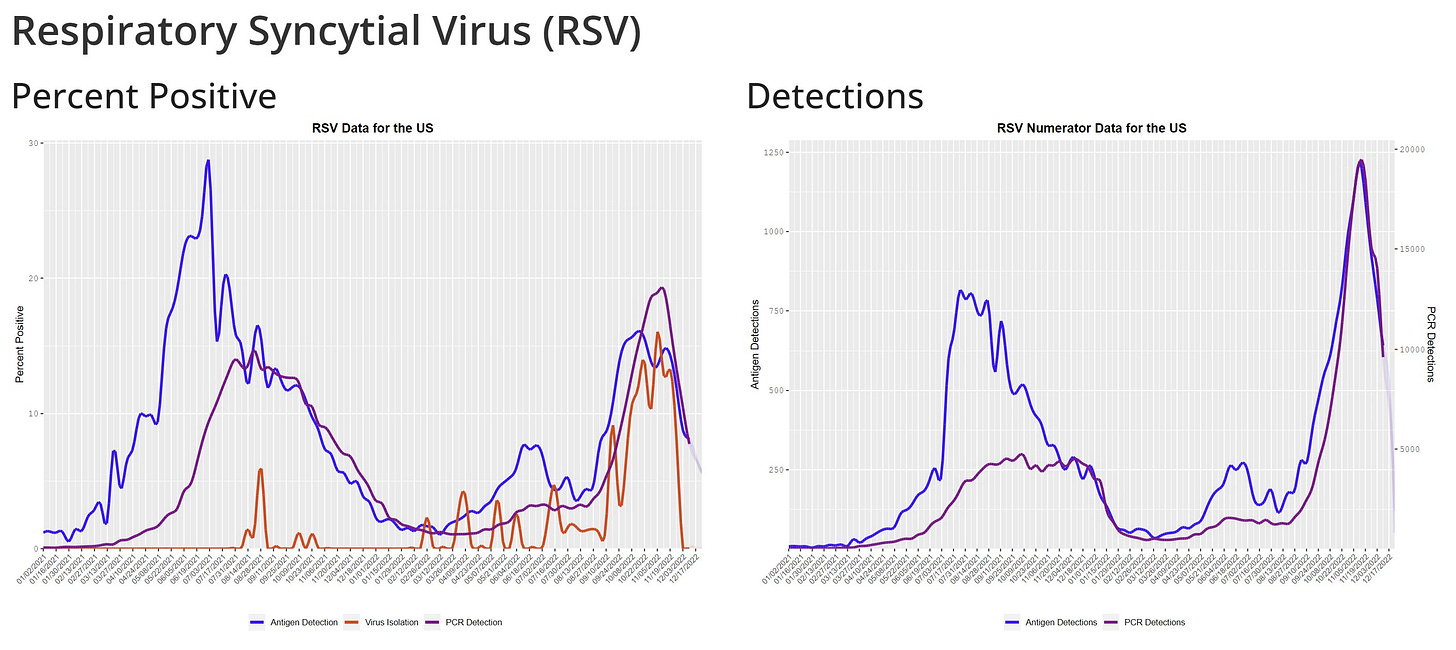
In mid-November 2022, at the peak of RSV, hospitalizations blew pre-pandemic years out of the water. This was mainly driven by admissions among kids under 5 years old, which reached an all time high rate of 70 kids hospitalized per 100,000 infections. (Historically, peaks range from 26-52 kids hospitalized per 100,000 infections).
Flu
Flu continues to follow RSV and is also trending downwards, but certainly not as quickly. All metrics—test positivity rate, positives in nursing homes, hospitalization—are showing reprieve.
As far as cumulative severity, the Northern Hemisphere is largely reflecting patterns of the Southern Hemisphere last summer—flu is back, but not particularly severe. Flu hospitalizations are on track for a mediocre season compared to, for example, the severe 2017-2018 flu season.
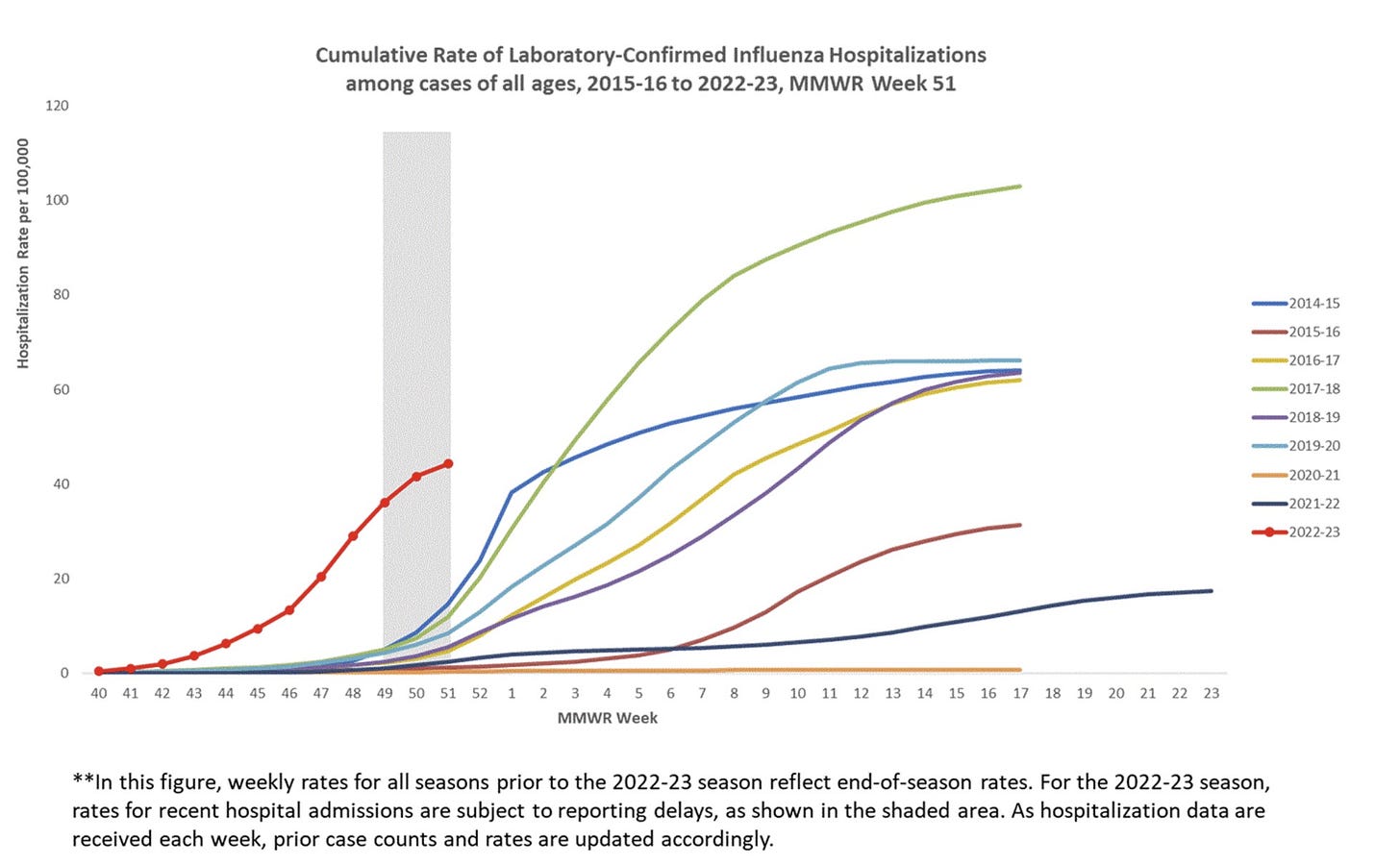
This doesn’t mean there isn’t any suffering, though. We have already lost 13,000 Americans to the flu—61 of those were children.
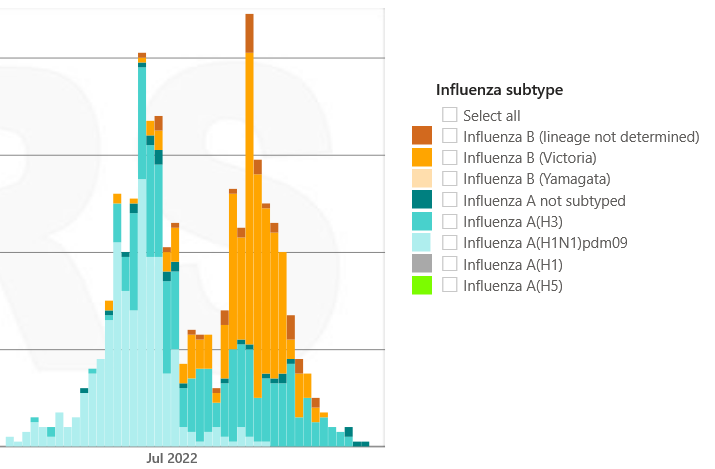
Will flu continue to decline? Not necessarily. Countries in the Southern Hemisphere, like South Africa, saw two waves of flu: the first driven by one strain—called influenza A—and the second driven by another strain—influenza B. Currently, influenza A is driving U.S. cases, which means that we, too, may have another wave.
COVID-19
Then there’s COVID, the only one of these three viruses trending upwards right now.
I’ll start with the good news: we got through 2022—one full year—without a new variant of concern. In other words, Omicron continued to mutate without a variant coming out from left field. As I’ve written before, this is a welcome development.
The bad news: Omicron subvariants continue to do plenty of damage on their own. This is especially the case when coupled with the holidays (i.e. changing behaviors and social networks) and cooler weather.
Currently the viral culprit is XBB.1.5., which has caught the attention of many. In fact, the WHO is currently conducting a risk assessment, which should be out in a few days.
XBB.1.5 continues to have a viral advantage in the U.S. as it started in the Northeast and is now quickly bleeding into the South and will soon dominate in the Midwest and West. A great visualization below displays the projected spread. A peak is expected in February.
A visualization of when spikes are expected in other parts of the country
4:01 AM ∙ Jan 4, 202361Likes9Retweets
How big or severe will the wave be?
It’s hard to predict given such a complex immunity wall in the U.S. and limited knowledge of XBB.1.5, including the inability to rely on trends from other countries, as this is a homegrown problem. (Singapore had a XBB wave, but XBB.1.5. is a 3-generation difference. Also, Singapore has a highly boosted population.)
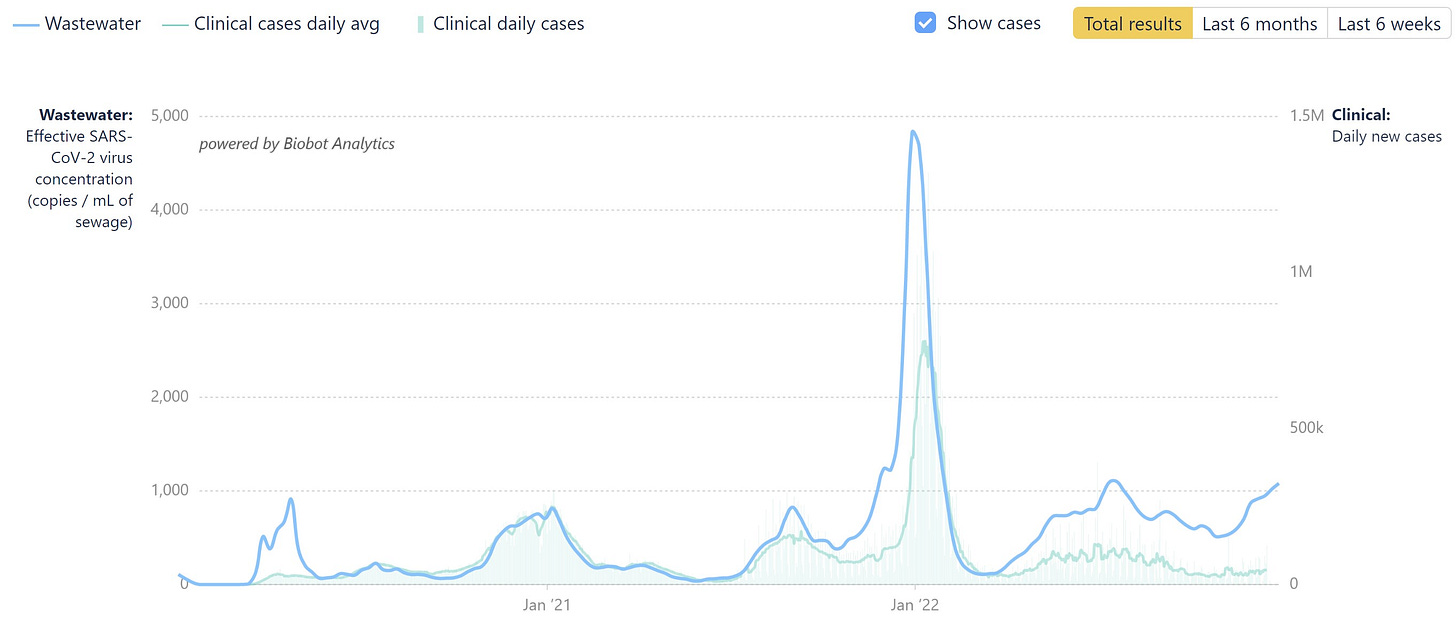
Regardless, we are already in a wave. For really the first time, reported case numbers have completely decoupled from wastewater, so we can’t rely on this anymore. Wastewater is clearly on the rise.
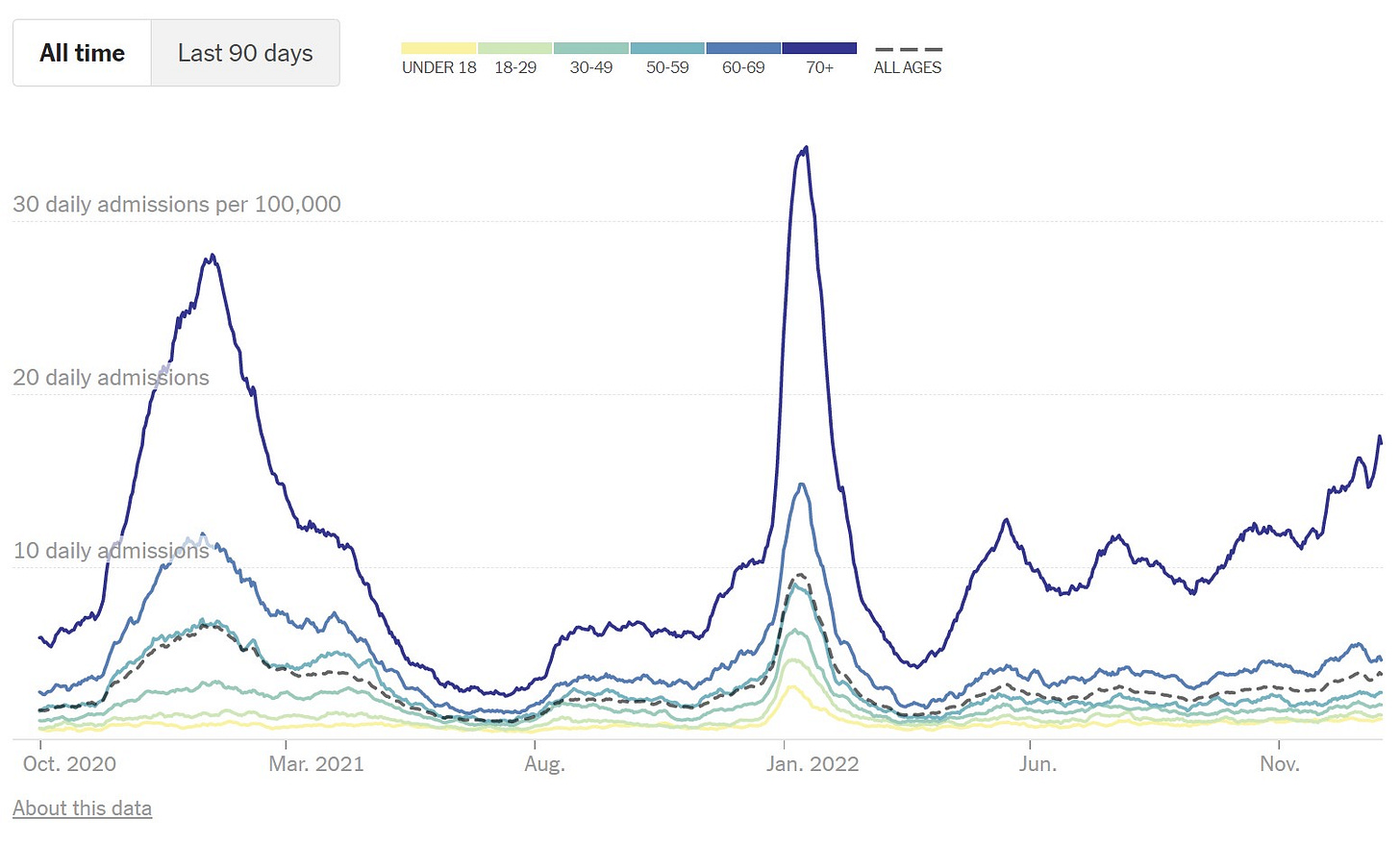
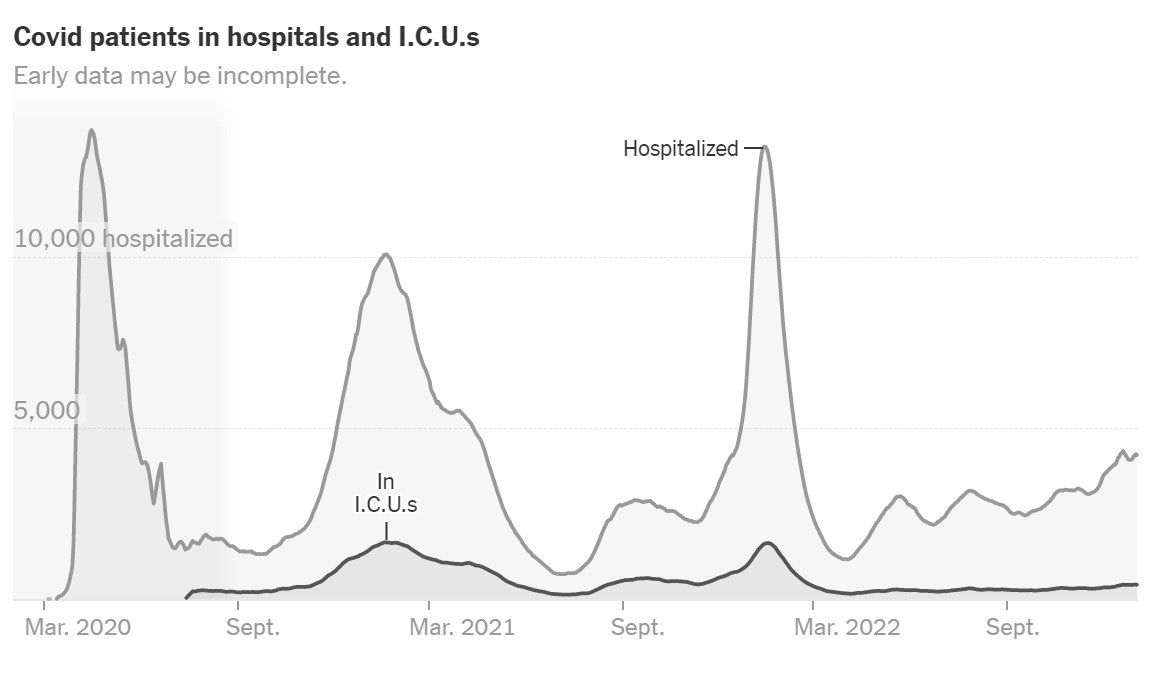
Unfortunately, hospitalizations are increasing too.
In the Northeast, hospitalizations among those over 70 years old are reaching very uncomfortable levels. They aren’t close to last winter, yet, but let’s please not make last winter’s disaster our standard of health.
It’s important to note two positive things regarding severe disease:
- Hospitalizations are very different today than they used to be. Indicators of severe hospitalization, like ICU use and proportions of dexamethasone administered— the standard of care for COVID-19 pneumonia—are not increasing.
- This is a good sign that the severity of Omicron with XBB.1.5 mutations may not have changed, but we don’t have hard evidence of this yet.
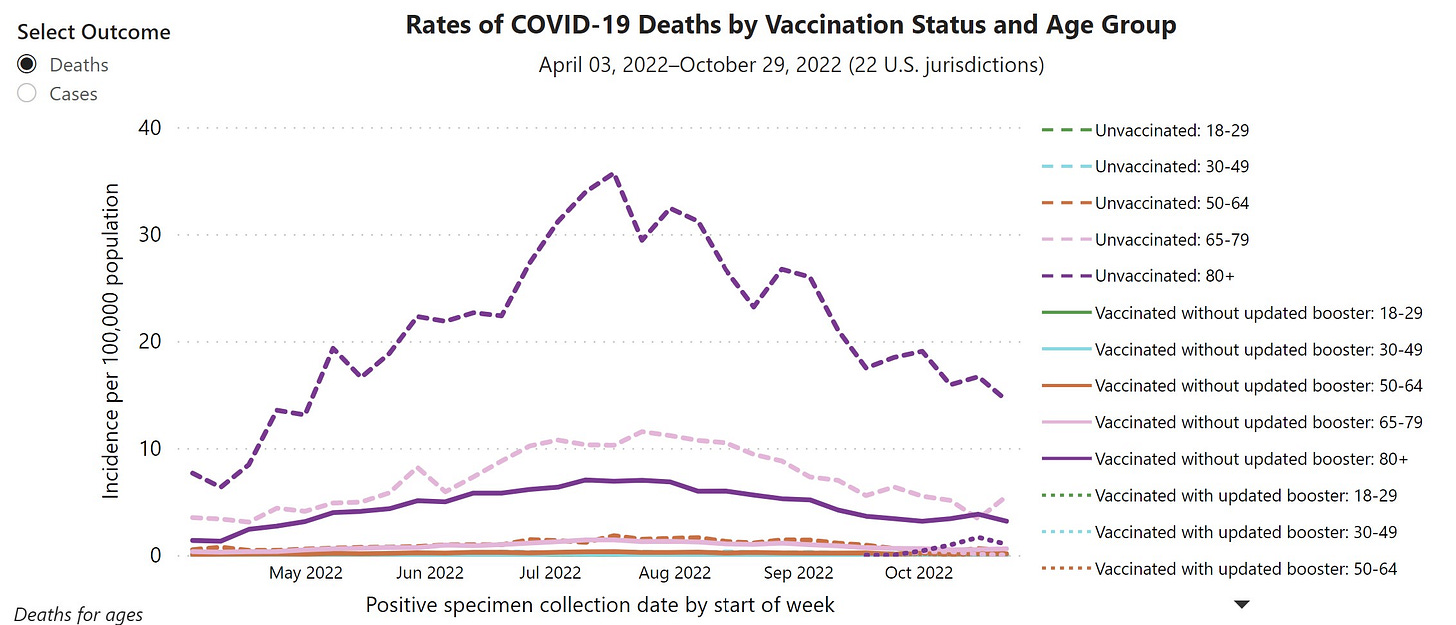
- Vaccines work. People vaccinated with the fall booster have an 18.6 times lower risk of dying from COVID-19 than unvaccinated people right now. The risk of infection is also three times lower. This is even the case for people with weaker immune systems, like those over 80 years old.
One of the biggest problems with the newer subvariants is that monoclonal antibodies, including Evusheild, do not work. (Paxlovid still works.)
This means that part of the safety net we had for the vulnerable is missing, which is a massive problem. Unfortunately, it looks like this will take months to fix.
Bottom line
RSV and flu trends are showing welcoming signs, but COVID-19 is now taking over.
The impact of XBB.1.5 and the height of the COVID-19 winter wave is unknown, but the vulnerable are already in a tough spot.
There are a lot of sick people out there and still plenty of winter season left. Stay healthy… You know what to do.
